Big COVIData Study: Predictive factors for the evolution of patients with COVID-19
Fill the form and join the study
Results of the Big COVIData Study
Here you can find the results of the first international study applying Big Data, Machine Learning, and Natural Language Processing to define the clinical characteristics and predictive factors for the evolution of patients with COVID-19 in English-, French-, German-, and Spanish-speaking countries conducted by Savana.
EVIDENCE OF GENDER DIFFERENCES IN THE DIAGNOSIS AND MANAGEMENT OF COVID-19 PATIENTS
Dec 16th, 2020
Abstract
- Background:
The impact of sex and gender in the incidence and severity of coronavirus disease 2019 (COVID-19) remains controversial. Here, we aim to describe the characteristics of COVID-19 patients at disease onset, with special focus on the diagnosis and management of female patients with COVID-19. - Methods:
We explored the unstructured free text in the electronic health records (EHRs) within the SESCAM Healthcare Network (Castilla La-Mancha, Spain). The study sample comprised the entire population with available EHRs (1,446,452 patients) from January 1st to May 1st, 2020. We extracted patients' clinical information upon diagnosis, progression, and outcome for all COVID-19 cases. - Results:
A total of 4,780 patients with a confirmed diagnosis of COVID-19 were identified. Of these, 2,443 (51%) were female, who were on average 1.5 years younger than male patients (61.7 ± 19.4 vs. 63.3 ± 18.3, p = 0.0025). There were more female COVID-19 cases in the 15–59-year-old interval, with the greatest sex ratio (95% confidence interval) observed in the 30–39-year-old range (1.69; 1.35–2.11). Upon diagnosis, headache, anosmia, and ageusia were significantly more frequent in females than males. Imaging by chest X-ray or blood tests were performed less frequently in females (65.5% vs. 78.3% and 49.5% vs. 63.7%, respectively), all p < 0.001. Regarding hospital resource use, females showed less frequency of hospitalization (44.3% vs. 62.0%) and intensive care unit admission (2.8% vs. 6.3%) than males, all p < 0.001. - Conclusion:
Our results indicate important sex-dependent differences in the diagnosis, clinical manifestation, and treatment of patients with COVID-19. These results warrant further research to identify and close the gender gap in the ongoing pandemic.
Read the complete study published in the Journal of Women's Health
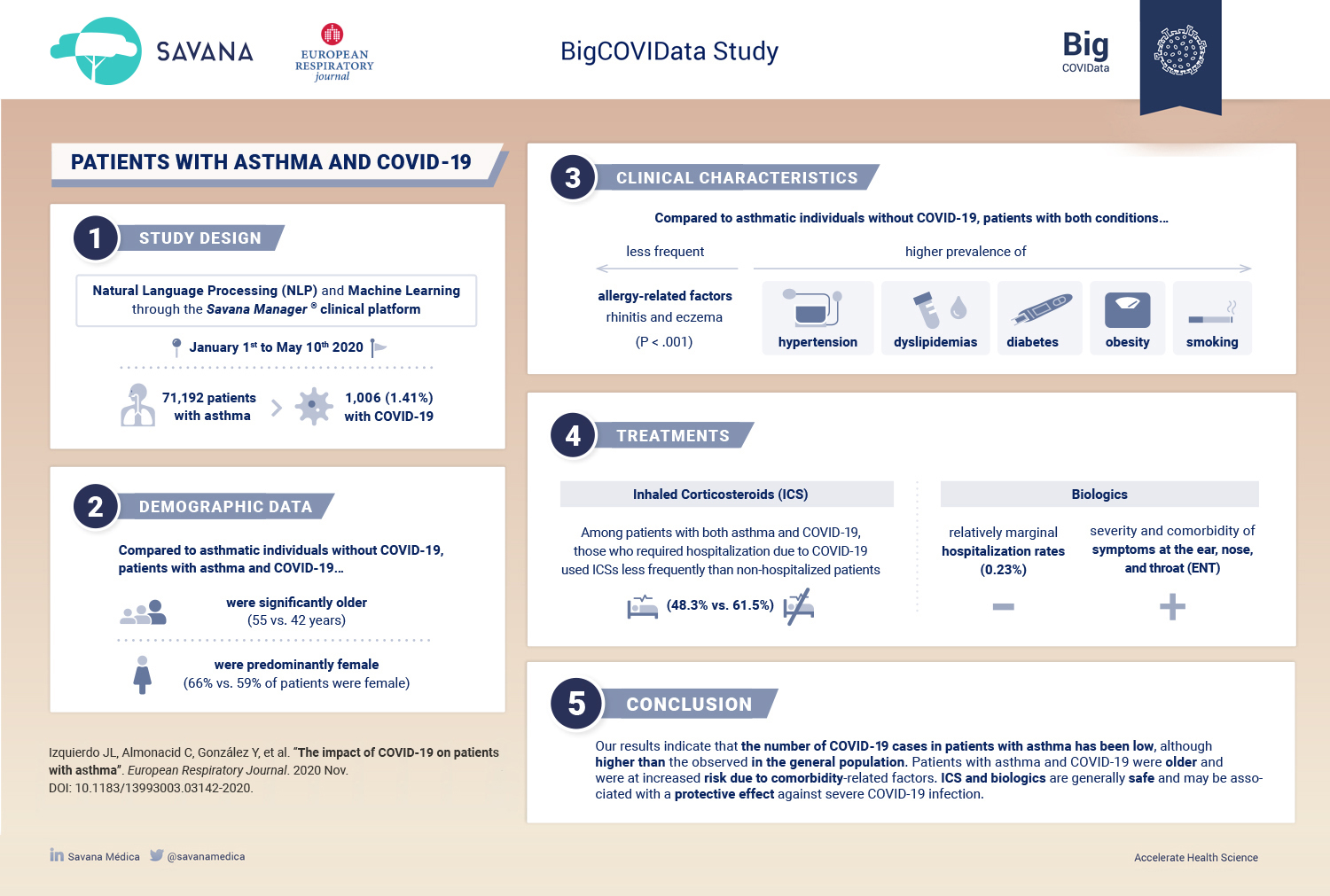
THE IMPACT OF COVID-19 ON PATIENTS WITH ASTHMA
November 5th, 2020
Abstract
- Background:
An association between the severity of COVID-19 and the presence of certain chronic conditions has been suggested. However, unlike influenza and other viruses, the disease burden in patients with asthma has been less evident. - Objective:
To understand the impact of COVID-19 in patients with asthma. - Methods:
Using big data analytics and artificial intelligence through the SAVANA Manager® clinical platform, we analysed clinical data from patients with asthma from January 1st to May 10th, 2020. - Results:
Out of 71 182 patients with asthma, 1006 (1.41%) suffered from COVID-19. Compared to asthmatic individuals without COVID-19, patients with asthma and COVID-19 were significantly older (55 versus 42 years), predominantly female (66% versus 59%), smoked more frequently, and had higher prevalence of hypertension, dyslipidemias, diabetes, and obesity. Allergy-related factors such as rhinitis and eczema were less common in asthmatic patients with COVID-19 (p<.001). Higher prevalence of these comorbidities was also observed in patients with COVID-19 who required hospital admission. The use of inhaled corticosteroids (ICS) was lower in patients who required hospitalisation due to COVID-19, as compared to non-hospitalised patients (48.3% versus 61.5%; OR: 0.58: 95% CI 0.44–0.77). Although patients treated with biologics (n=865; 1.21%) showed increased severity and more comorbidities at the ENT level, COVID-19-related hospitalisations in these patients were relatively low (0.23%). - Conclusion:
Patients with asthma and COVID-19 were older and at increased risk due to comorbidity-related factors. ICS and biologics are generally safe and may be associated with a protective effect against severe COVID-19 infection.
Read the complete study published in the European Respiratory Journal.
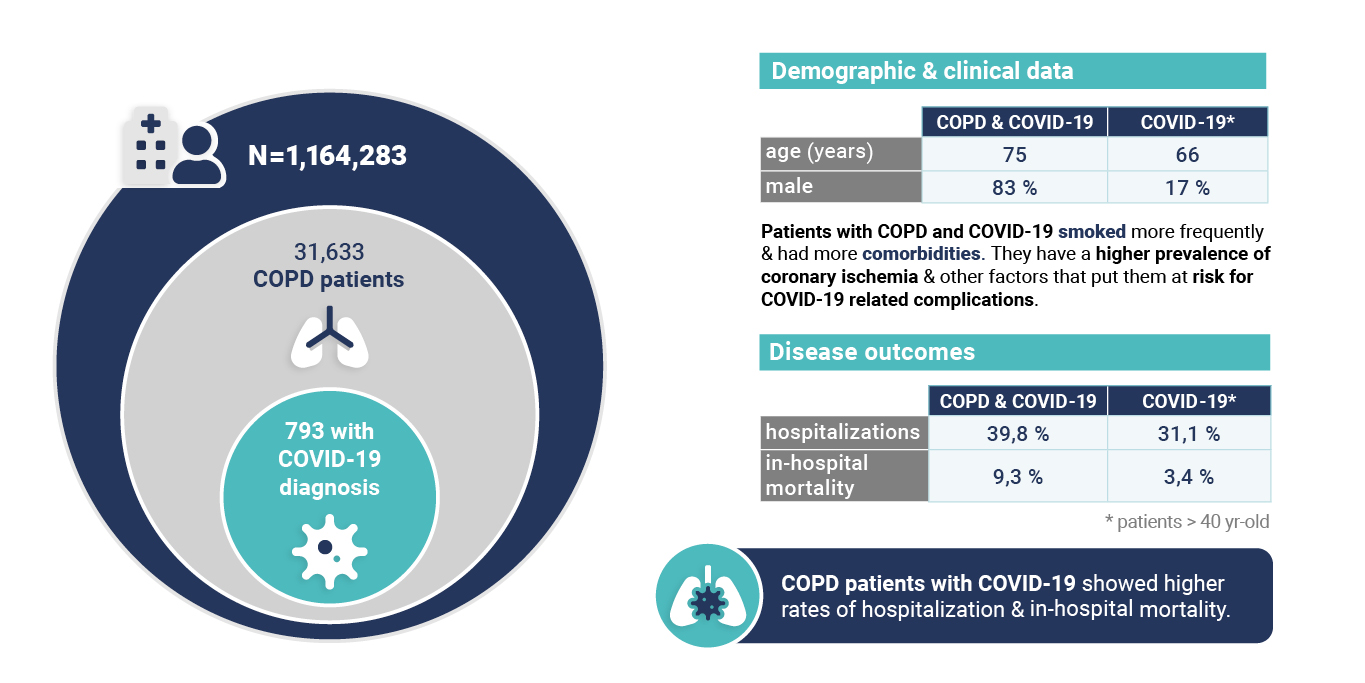
CHARACTERISTICS AND PROGNOSIS OF COVID-19 IN PATIENTS WITH COPD
Oct 12th, 2020
Abstract
Patients with Chronic Obstructive Pulmonary Disease (COPD) have a higher prevalence of coronary ischemia and other factors that put them at risk for COVID-19-related complications. We aimed to explore the impact of COVID-19 in a large population-based sample of patients with COPD in Castilla-La Mancha, Spain.We analyzed clinical data in electronic health records from 1 January to 10 May 2020 by using Natural Language Processing through the SAVANA Manager® clinical platform. Out of 31,633 COPD patients, 793 had a diagnosis of COVID-19. The proportion of patients with COVID-19 in the COPD population (2.51%; 95% CI 2.33–2.68) was significantly higher than in the general population aged > 40 years (1.16%; 95% CI 1.14–1.18); p < 0.001. Compared with COPD-free individuals, COPD patients with COVID-19 showed significantly poorer disease prognosis, as evaluated by hospitalizations (31.1% vs. 39.8%: OR 1.57; 95% CI 1.14–1.18) and mortality (3.4% vs. 9.3%: OR 2.93; 95% CI 2.27–3.79).
Patients with COPD and COVID-19 were significantly older (75 vs. 66 years), predominantly male (83% vs. 17%), smoked more frequently, and had more comorbidities than their non-COPD counterparts. Pneumonia was the most common diagnosis among COPD patients hospitalized due to COVID-19 (59%); 19% of patients showed pulmonary infiltrates suggestive of pneumonia and heart failure. Mortality in COPD patients with COVID-19 was associated with older age and prevalence of heart failure (p < 0.05). COPD patients with COVID-19 showed higher rates of hospitalization and mortality, mainly associated with pneumonia. This clinical profile is different from exacerbations caused by other respiratory viruses in the winter season.
Read the complete study published in the Journal of Clinical Medicine.
Read the complete study published in the Journal of Clinical Medicine.
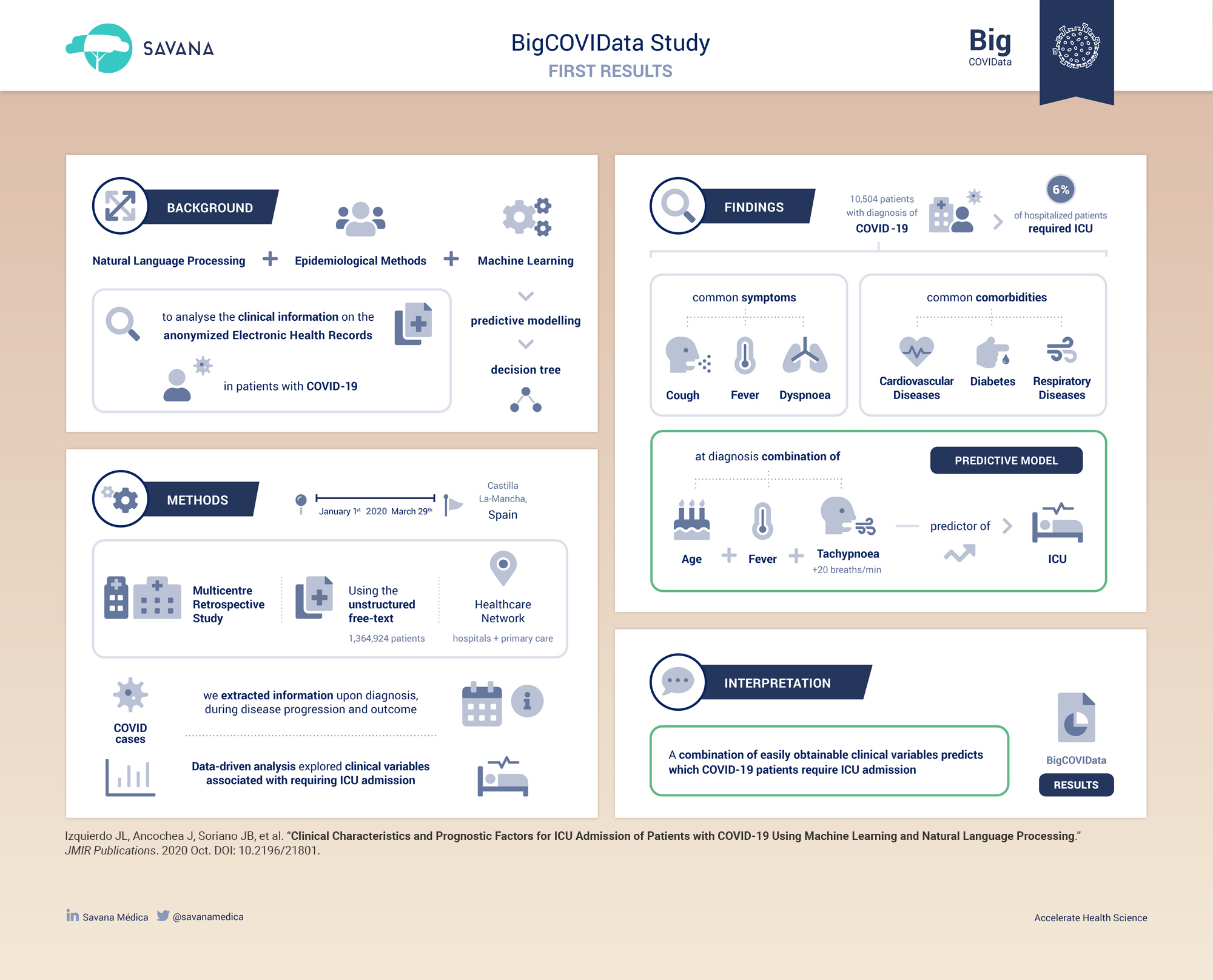
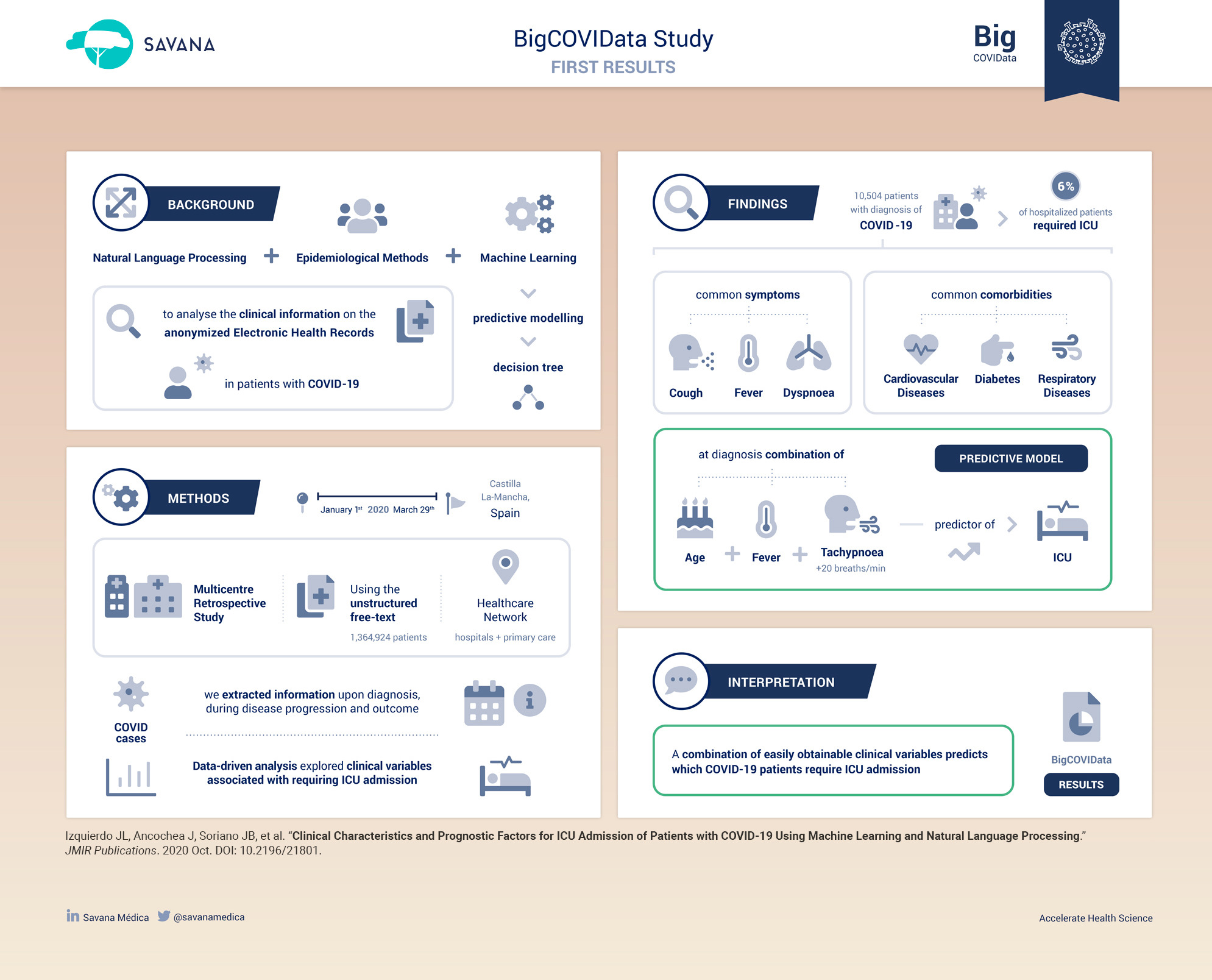
CLINICAL CHARACTERISTICS AND PROGNOSTIC FACTORS FOR ICU ADMISSION OF PATIENTS WITH COVID-19
Oct 28th, 2020
Abstract
- Background:
Many factors involved in the onset and clinical course of the ongoing COVID-19 pandemic are still unknown. Although big data analytics and artificial intelligence are widely used in the realms of health and medicine, researchers are only beginning to use these tools to explore the clinical characteristics and predictive factors of patients with COVID-19. - Objective:
Our primary objectives are to describe the clinical characteristics and determine the factors that predict intensive care unit (ICU) admission of patients with COVID-19. Determining these factors using a well-defined population can increase our understanding of the real-world epidemiology of the disease. - Methods:
We used a combination of classic epidemiological methods, natural language processing (NLP), and machine learning (for predictive modeling) to analyze the electronic health records (EHRs) of patients with COVID-19. We explored the unstructured free text in the EHRs within the Servicio de Salud de Castilla-La Mancha (SESCAM) Health Care Network (Castilla-La Mancha, Spain) from the entire population with available EHRs (1,364,924 patients) from January 1 to March 29, 2020. We extracted related clinical information regarding diagnosis, progression, and outcome for all COVID-19 cases. - Results:
A total of 10,504 patients with a clinical or polymerase chain reaction–confirmed diagnosis of COVID-19 were identified; 5519 (52.5%) were male, with a mean age of 58.2 years (SD 19.7). Upon admission, the most common symptoms were cough, fever, and dyspnea; however, all three symptoms occurred in fewer than half of the cases. Overall, 6.1% (83/1353) of hospitalized patients required ICU admission. Using a machine-learning, data-driven algorithm, we identified that a combination of age, fever, and tachypnea was the most parsimonious predictor of ICU admission; patients younger than 56 years, without tachypnea, and temperature <39 degrees Celsius (or >39 ºC without respiratory crackles) were not admitted to the ICU. In contrast, patients with COVID-19 aged 40 to 79 years were likely to be admitted to the ICU if they had tachypnea and delayed their visit to the emergency department after being seen in primary care. - Conclusions:
Our results show that a combination of easily obtainable clinical variables (age, fever, and tachypnea with or without respiratory crackles) predicts whether patients with COVID-19 will require ICU admission.
Read the complete study published in the Journal of Medical Internet Research.
Request more information

AI + RWE
Savanamed.com © 2019 | Legal notice | Privacy policy | Cookies Policy


